What is Evidence-Based Practice and Why Is It Important?
Written by Eric Lazar FMS
Although it’s roots can be traced back earlier in history,[1] Evidence-Based Medicine (EBM) was first introduced by Dr. Gordon Guyatt of McMaster University in Canada to the publishing world when it appeared in the Journal of the American Medical Association in 1992.[2] In the subsequent years numerous publications were released that better defined what EBM (or “EBP” for “Evidence-Based Practice”) was all about, including a seminal article by Sackett et al in 1996.[3]
One of the most common misconceptions about EBP is that it is strictly about research. However, there are 3 major components, each of equal importance, that formulate this concept:
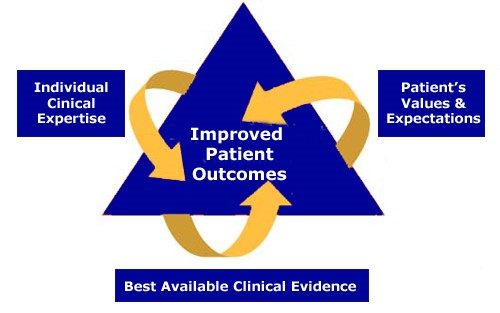
The diagrams show that “best research evidence” is one of the major players of EBP, the other two being clinical expertise and patient values (also reported as “preferences” or “expectations”). It is the combination of these 3 elements that leads to the ultimate goal of improved patient/client outcomes. A problem many fitness and healthcare professionals continue to have is to rely exclusively on their expertise in the field, and not take into account patient/client preferences and the most up-to-date research.
Too often, clinical or program planning decisions are based more on tradition than solid science. For example, many strength and conditioning and rehabilitation professionals have traditionally recommended rest, ice, compression and elevation (RICE) following an acute ankle sprain, but the evidence is inconclusive about the relative effectiveness of RICE.[4] In fact, an editorial suggested that new guidelines incorporate “POLICE” (P = “Protection” and OL = “Optimal Loading”) to pave the way for more research on this subject.[5]
There are many forms of research that fitness and rehabilitation professionals need to understand to make informed decisions about client/patient care. Presently the highest forms of evidence for making such decisions come from clinical guidelines or systematic reviews based on randomized controlled trials (RCTs). The word “controlled” refers to the need to control for bias. All professionals are subject to applying bias in their day to day work. For example, if you just attended a course on a new strengthening or treatment technique, there is a good chance you will be biased toward applying this newly acquired information on many clients/patients, even though that technique may not be appropriate in some cases.
The typical RCT compares an experimental group to a control group. In a recent study of overweight adults with metabolic syndrome,[6] two different weight loss programs were compared: the control group subjects were provided with body weight scales and pedometers, while the experimental group subjects were provided with remote body composition monitors and pedometers. It turns out that nearly all parameters measured in relation to weight loss were significantly better in the experimental group relative to the control group. Such a study could be helpful to a fitness or healthcare professional in making an informed decision on patient/client management of weight loss.
The type of study that appears most frequently in the FMS research is on reliability. Both intra-rater and inter-rater reliability of the Functional Movement Screen have been studied. Intra-rater reliability refers to the same tester’s ability to reproduce similar results on repeated tests. Inter-rater reliability refers to different testers’ ability to reproduce similar results on repeated tests. Generally, intra-rater reliability tends to be better since it is usually easier for the same examiner to obtain similar results than it is for a group of different examiners to have comparable outcomes. Fortunately in the case of the Functional Movement Screen, both intra-rater and inter-rater reliability have been shown to be good to excellent.[7]
Many studies have also looked at the Functional Movement Screen for predicting risk of injury, most often based on the composite score. Frequently the terms sensitivity and specificity are used to predict serious injury based on the composite scores of the Functional Movement Screen. Sensitivity looks at a test’s ability to detect a disease or condition. If a test is highly sensitive, and the test result is negative, you can be almost certain that the person being tested does not have the condition in question. Therefore, the mnemonic SnOut is used: a highly Sensitive test rules out the presence of disease. In the case of the Functional Movement Screen, high sensitivity helps rule out people at risk of musculoskeletal injury. Specificity looks at a test’s ability to detect those who do not have a disease or condition. If a test is highly specific, and the test result is positive, you can be almost certain that the person being tested does have the condition in question. Therefore, the mnemonic SpIn is used: a highly Specific test rules In the presence of disease. In the case of the Functional Movement Screen, high specificity helps rule in people at risk of musculoskeletal injury.
While the data is mixed on sensitivity and specificity statistics of the Functional Movement Screen,7 it must be reiterated that the Functional Movement Screen was never meant to be an injury prediction tool in and of itself, but an adjunct to a battery of other tests used for assessing injury risk. In fact, the recent study by Teyhen et al [8] showed high sensitivity (0.90) and high specificity (0.98) when taking into account several risk factors for musculoskeletal injury. Such research combining multiple risk factors can help health and fitness professionals make better decisions for those who may (or may not) be at greater risk of suffering a musculoskeletal injury. Please refer to the detailed research review by Phil Plisky for more in-depth information.

[1] Smith R, Rennie D. Evidence-based medicine--an oral history. JAMA. 2014 Jan 22-29;311(4):365-7.
[2] Evidence-Based Medicine Working Group. Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420-2425.
[3] Sackett DL, Rosenberg WMC, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71-72.
[4] Van den Bekerom MP et al. What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults?
[5] Bleakley CM, Glasgow P, MacAuley DC. PRICE needs updating, should we call the POLICE? Br J Sports Med. 2012:46:220-221.
[6] Oh B et al. The effectiveness of mobile phone-based care for weight control in metabolic syndrome patients: randomized controlled trial. JMIR Mhealth Uhealth. 2015 Aug 20;3(3):e83.
[7] Kraus, K., E. Schutz, W. R. Taylor and R. Doyscher (2014). Efficacy of the functional movement screen: a review. J Strength Cond Res 28(12): 3571-3584.
[8] Teyhen, D. S., S. W. Shaffer, R. J. Butler, S. L. Goffar, K. B. Kiesel, D. I. Rhon, J. N. Williamson and P. J. Plisky (2015). What risk factors are associated with musculoskeletal injury in US Army Rangers? A prospective prognostic study." Clin Orthop Relat Res 473(9): 2948-2958.
Related Resources
-
Start With Why
Posted by Gray Cook
-
Preventing Sports Injuries
Posted by Byron Rohrig
-
Revisiting Athletic Body in Balance
Posted by Gray Cook
Please login to leave a comment
2 Comments
-

Ramon Sodano 12/14/2015 1:53:54 PM
Ha, this is awesome you guys just posted this. I just finished running my initial statistics on the FMS as an injury predictor in my meta-analysis. Still ironing out quite a few aspects which the moderator analyses will shed a lot more light onto, however. I will let you all know more when I get completely done. I will say the overall Odds Ratio is in your favor, but it is not as large as claimed in Kiesel's 2007 NFL study. Regardless, it is difficult to run a meta-analysis on this topic for many reasons but two main ones are the fact that half the research utilized a cut off score of 14 as suggested from previous research and others used ROC curve analysis to identify a score threshold with regard to maximizing sensitivity and 1-spefcecity. Another large obstacle (among a few others) was the various definitions of what injury was. When coding for these I came up with 7 different definitions that encapsulated the definitions in the studies included in the meta-analysis. However, there are 13 studies (one study has two sub groups though) so 14 total pieces of data utilized for 7 definitions of injury. It should be noted that most could be included in one of the definitions, and the others varied quite a bit. However, when running moderator analysis’s on these concepts (among others) will shed more light on to what we are looking at. Again, ill keep ya’’ informed. I realize that meaning of the FMS was not to be an injury predictor, but if we can find some data on its usefulness with regard to this it could be extremely beneficial.
-

Ronnie Depesa 1/8/2016 4:54:12 PM
@ramon sodano: good points and I find your take on what is an injury (classifications or definitions?) interesting.