The Relationship Between the FMS and Injury Risk
Written by Phil Plisky FMS
Is the Functional Movement Screen Reliable?
Currently, there are over 14 reliability studies on the Functional Movement Screen that indicate that it has good to excellent reliability. From systematic reviews, it is apparent that the reliability is better when the rater has more experience with and is Certified in the Functional Movement Screen.
In a systematic review of 12 Functional Movement Screen reliability articles, the authors state “There is a ‘moderate’ level of evidence in favor of acceptable inter-rater and intra-rater reliability for composite scores derived from live scoring. Ratings made from live observation were superior to those made from viewing of video recordings. Moran et al BJSM 2015
“On the descriptive level, results suggest that the FMS is a reliable screen, if the rater is educated and has solid experience (greater than 100 trials).” Kraus et al J Strength Cond Res 2014
Functional Movement Screen & Relationship to Injury

Before we dive into discussing some misconceptions about the Functional Movement Screen, let’s start with a few principles so we’re on the same page.
When the first research was done on the Functional Movement Screen, it was clinically noted that athletes who scored 14 or below tended to get injured more than those that scored higher. While the Functional Movement Screen composite score was initially used in injury prediction research, the raw score on the individual tests is more important. That is to say, you should not have any 0’s (pain) or 1’s (can’t perform a fundamental movement pattern) on any individual test. But guess what, if you have at least 2’s on all 7 tests, you already have a minimum of a 14 - which might explain why the composite score of 14 has received so much attention.
Remember, the Functional Movement Screen is a filter. What are you trying to catch with this filter? We are primarily interested in catching pain with movement as well as the complete inability to perform a fundamental movement pattern.
The purpose of the Functional Movement Screen is to:
- Set a movement baseline
- Identify major problems with basic movement patterns
What are major problems? In order of priority, they are:
- Pain with movement (scored as a 0 on the Functional Movement Screen)
- Inability to perform a simple movement pattern even when allowed a compensation (score of a 1 on test)
- Major asymmetry with movement
We also need to remember that the Functional Movement Screen is PART of a system that includes a movement-based diagnostic assessment performed by healthcare providers (Selective Functional Movement Assessment) if there is pain or injury as well as testing designed to examine functional symmetry (Y Balance Test Upper and Lower Quarter).
Is the Functional Movement Screen a good screen? Our immediate question should be: “For what purpose?”
- Screening an athlete for risk of injury? Not always by itself. It’s best to use multiple factors (see how this has been researched below). If it’s positive by itself, it warrants further investigation and/or treatment, particularly if pain is present.
- Identifying someone who has pain during 7 basic movements? Yes, pain with basic movement patterns has been identified as a risk factor by multiple studies
- Identifying a person who is unable to perform 7 basic movement patterns? Yes
As summarized in this table, eleven studies found some relationship with FMS and injury in American Professional Football, collegiate athletes, military officer candidates, US army rangers, firefighters, and male competitive runners (ages 18 – 24). Four studies (table) did not find an association between FMS and injury. Two of those studies had substantially flawed methodology (see comments). In meta-analysis completed by Dorrel et al (2015), the FMS provides adequate specificity (85%) and low sensitivity (24%). This basically means that if you have a low FMS score, you are more likely to get hurt. However, having a high FMS score does not protect you from injury.
Research Validation of Application of the Functional Movement System in Injury Prediction in Collegiate Athletes
Since the Functional Movement Screen was not intended to be the ONLY factor used in injury prediction (current research clearly tells us that injury risk is multi-factorial) Lehr et al used the Move2Perform injury prediction algorithm to categorize injury risk using components of the Functional Movement System. This went beyond simply looking at the FMS composite score.
The following evidence-based components (risk factors) with various weightings and interactions were included in the algorithm:
- Previous Injury
- Y Balance Test Composite risk cut score based on sex, sport, and competition level
- Y Balance Test Asymmetry
- Functional Movement Screen Total Score
- Functional Movement Screen Asymmetry
- Pain with testing
Here are the results of that study (Lehr 2013)
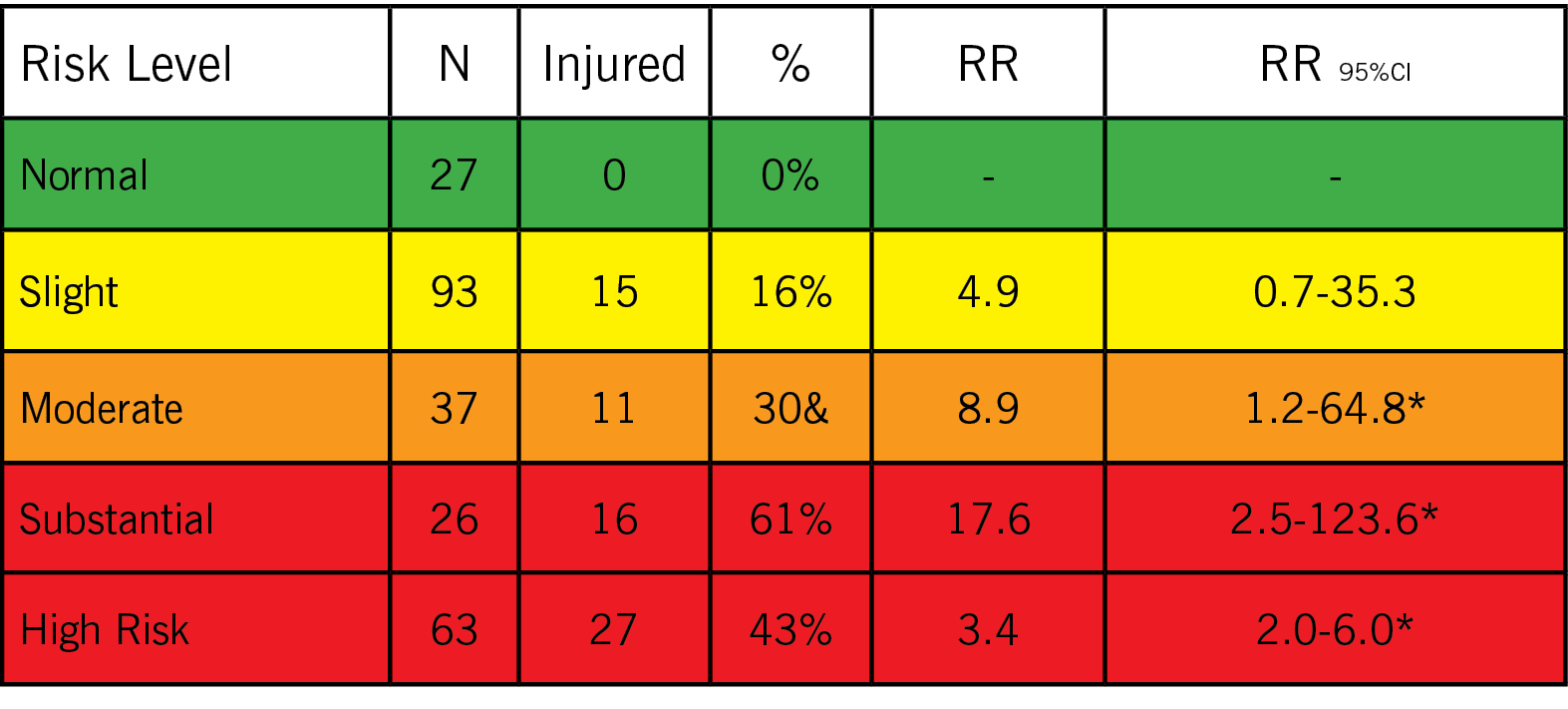
When multiple risk factors are used in combination, the injury prediction results become more robust. To give an example of how the algorithm categorizes athletes:
- Those in the high-risk categories were nearly 3.5 times more likely would have pain with testing or previous injury with a Y Balance Test Composite below the risk cut score based on sex, sport, and competition level; no Y Balance Test Asymmetry; Functional Movement Screen Total Score above 14; and no Functional Movement Screen Asymmetry.
- Those in the low-risk categories would not have a previous injury, a Y Balance Test Composite above the risk cut score based on sex, sport, and competition level; no Y Balance Test Asymmetry; Functional Movement Screen Total Score above 14; no Functional Movement Screen Asymmetry, and no pain with testing.
Bottom Line: Professionals should utilize multiple risk factors and weigh those factors when determining and managing individual injury risk. Using a multifactorial injury risk algorithm that weights pain first and then multiple aspects of other factors such as (Injury History, Functional Movement Screen, Y Balance Test Lower Quarter) is recommended. Intervention and resources should be matched to the appropriate category.
*Note that researchers have found that being in the Normal Risk Category may be a protective factor for injury. Striving for this category is a worthwhile goal.
Injury Risk Categories:
1) Substantial Deficit
There is pain with testing (injury) or substantial dysfunction. This requires one on one evaluation (Selective Functional Movement Assessment) and intervention with a health-care provider. Re-testing to ensure lower category is key.
2) Moderate Deficit
Depending on your medical history (likely to get injured and no one in the normal group was injured (high sensitivity = 1.0).
To be clear, someone in the normal category had an injury/surgery recently or multiple injuries?) and your current circumstances, you need one on one intervention with either a strength and conditioning or medical professional. Re-testing to ensure lower category is key.
3) Slight Deficit
This is a warning sign, you may not require one on one intervention, but you should be actively working with your medical and strength and conditioning professional, modifying your lifestyle, and re-testing regularly.
4) Optimal
Keep up the good work. Continue with evidence-based group injury prevention programs. You still need regular monitoring of your risk factors.
The Functional Movement Screen results relate to how the person will perform under load or in competition.
Remember, the goal of the Functional Movement Screen is not to measure sport performance. So the research studies that are trying to see if it relates to performance really don’t make much sense. It is similar to looking at your RPMs on your tachometer. Physical and sport performance is also highly variable, so it’s difficult to compare athletes of different skill levels. One study did find a relationship of the Functional Movement Screen score and the potential for performance improvement in elite track and field athletes (Chapman et al 2013). If you have a quality foundation, you may be able to build better performance given the presence of that quality foundation.
Further, if someone does indeed pass the Functional Movement Screen and Y Balance Test, that he/she can still be at risk of injury because of poor landing mechanics, strength, endurance, poor agility, or power. Evidence-based group injury prevention programs can be highly effective for this person. Also, if he/she has passed, at least you can know that he/she possesses the basic motor control that makes in possible to improve those higher-level performance measures that they are striving to achieve.
Summary
Many of the misconceptions about the Functional Movement Screen relate to using a tool to perform something it was never designed to do. The FMS was not designed to:
- By itself be a comprehensive system for injury risk
- Determine a medical diagnosis or precisely pinpoint where the problem is
- Be used as a direct performance metric
For more on FMS Research - Check out Dr. Rob Butler with
"What the Research Tells us about the Functional Movement Screen"
Related Resources
-
Movement Principle # 9
Posted by Gray Cook
-
The Value of Self-Limiting Exercise
Posted by Gray Cook
Please login to leave a comment
5 Comments
-

B. Dale 12/14/2015 1:54:31 PM
We get it all the time from our officers during FMS screens...they score a 10 but then comment that they haven't missed a sick day in 2 years, 3 years and so forth. The missing link being of course that they don't actually participate in any fitness activities where they are at risk of injury.
Additionally our follow-up for low scores has been decidedly absent in that they are sent an email with attached PDF stretches to improve their score. The only stretch is then the employee reaching over to hit the delete key.........
-

-

Qiao Ming 2/29/2016 2:06:40 PM
Good article!
-
Thomas Padilla 3/8/2018 10:31:37 AM
I am a practicing SFG and FMS instructor, 1st off, reading this article has been great. I would love some insight though from anyone with a valid experience to share specifically utilizing FMS with their local fire department/Police/EMS etc. I am very much so wanting to present this system to them but i am filing through old and semi old "Studies" that sometimes have contradicting information.... anywho, i would love some insight from someone at FMS or someone with a direct experience, on how they think i can successfully approach and present myself as well as this system to these First Responder Departments in my area Thanks in Advance! Thomas SFG,FMS (210)241-5756
Drew Nelson, PT, DPT, CSCS, CES, FMSC, USAW ASPC 11/14/2018 7:42:58 PM
Hi Thomas, did you ever get anyone to contact you regarding your questions? Did you end up contacting your First Responder departments? How successful were things? I currently planning a similar endeavor with my local fire/police/EMS departments.