Breaking The Cycle
Written by Michele Desser SFMA
The journey through our professional careers is a continuous process of learning and honing our skills. We become more comfortable with our abilities while pursuing greater knowledge and understanding of the human body and how we can affect positive change. This journey has it’s ups and downs. Moments of defeat and moments of success. We can strive for perfection, but what makes us great is the drive to understand why something did not work and the willingness to move out of our comfort zones to find a solution.
I’ve been blessed to be surrounded by mentors who have instilled in me the need to be a problem solver. To look at each person in my care as an individual human being, not as a diagnosis. They taught me to avoid the trap of just treating someone’s pain. Instead, step back and see why that region is painful. They taught me to find the cause of someone’s pain, not just the source. Most importantly, they not only taught me, but showed me, diagnostics are the key to success. You can be the best manual therapist and have every tool available, but if it is not used in the right place, it will not be effective.
This key concept of proper diagnostics recently brought me both satisfaction, but also much frustration.
I had an individual reach out to schedule an assessment based on a referral from a former client. For the sake of privacy, I have changed her name to Mary for this article. In our initial phone conversation, Mary disclosed I would be the eighth healthcare professional she was seeing for her low back/SI pain. She also shared the hopelessness she felt with her situation. I couldn’t help but feel for Mary and the impact this condition was having on her life – I’ve been there myself. Pain like this causes a multitude of problems, not all physical.
At our initial assessment, Mary brought her list of priorly seen providers, her imaging results, and everything she has tried to mitigate the pain. We discussed her previous injury history – a right shoulder injury after falling off her bike years ago and multiple left ankle sprains. She is an active person and relies on exercise as a stress reliever. She currently is not able to exercise without increasing her pain levels. Simply talking about her experience caused Mary to become emotional as she again expressed hopelessness and that she has been made to feel it is “in her head”.
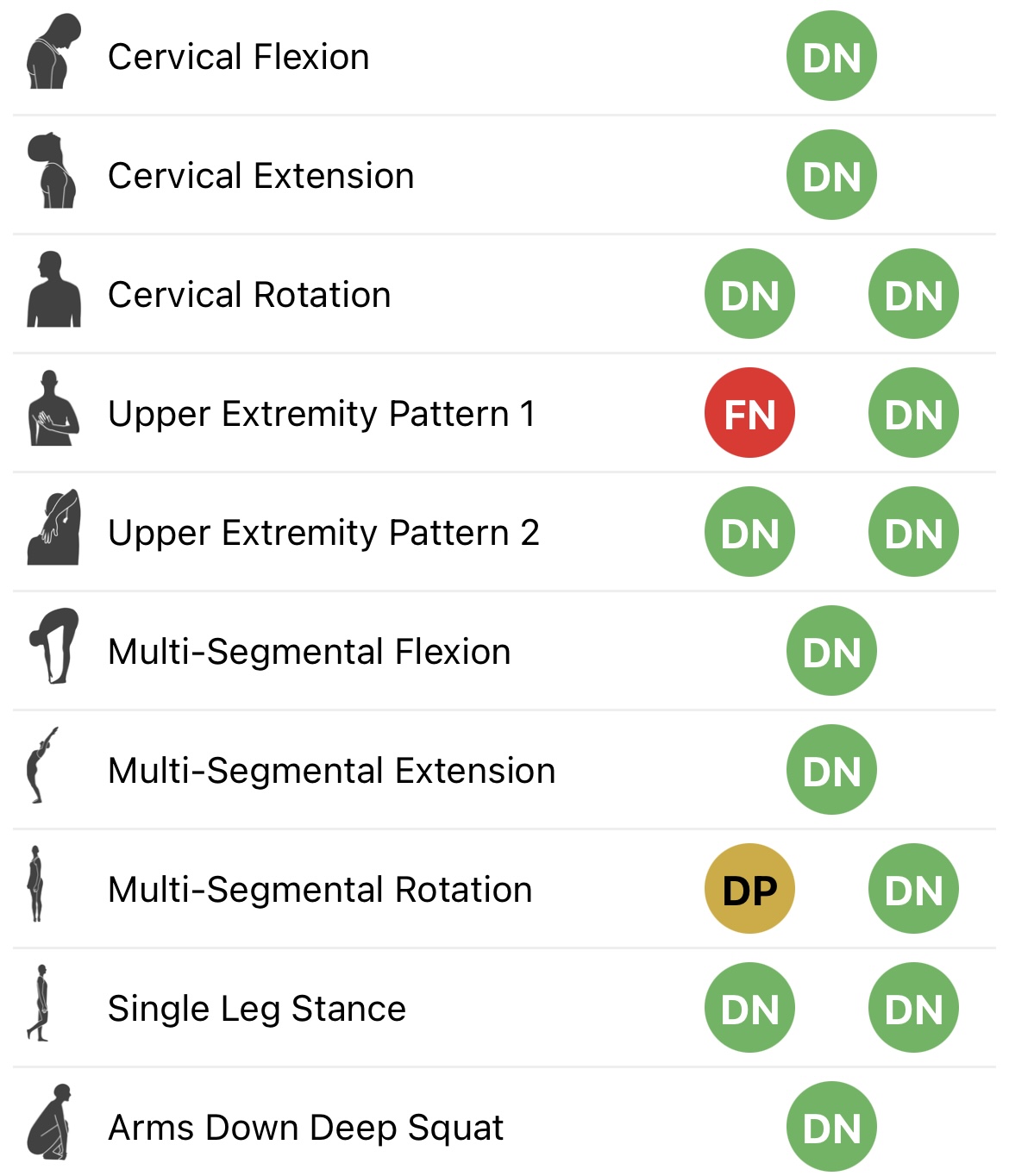 I began my assessment exactly the same way I begin every assessment – I performed the Selective Functional Movement Assessment (SFMA). I did not let any personal biases or assumptions interrupt my standard operating procedure. I looked at the Top Tier patterns and let those guide me to the appropriate breakouts. It was no shock that almost all the Top Tier patterns were dysfunctional, with Multi-Segmental Rotation to the left provoking pain. I needed to then breakout out all the dysfunctional patterns to tease out the biggest stressors to her system.
I began my assessment exactly the same way I begin every assessment – I performed the Selective Functional Movement Assessment (SFMA). I did not let any personal biases or assumptions interrupt my standard operating procedure. I looked at the Top Tier patterns and let those guide me to the appropriate breakouts. It was no shock that almost all the Top Tier patterns were dysfunctional, with Multi-Segmental Rotation to the left provoking pain. I needed to then breakout out all the dysfunctional patterns to tease out the biggest stressors to her system.
- Bilateral thorax ext/rot mobility restriction (right: 15 degrees, left: 30 degrees)
- Left ankle DF, eversion, and PF mobility restrictions
- Left tibial IR mobility restriction
-
Every clinician she has seen previously treated her low back and SI with no appreciable change to her symptoms. Knowing this ahead of time certainly gave me insight and an advantage. Even with this knowledge, I still followed my SOP to make sure I wasn’t guessing. The SFMA showed that her biggest issue was in her thorax, not her lumbar region! On top of that, there was a significant asymmetry in motion.
-
Mary’s hips had also been a focus for mobility interventions from many of the clinicians she worked with prior, but I identified that her hips actually moved quite well passively. She has adequate ROM. If anything, we could shift focus to motor control retraining of the hips.
-
She had been prescribed orthotics for her shoes. Within the SFMA, I identified a left ankle that was not moving appropriately. Mary was given a stability correction on an already immobile ankle. Her system had to break down somewhere!
- The biggest predictor of injury is previous injury. Her SFMA findings were lining up exactly to where her previous injuries had been – thorax, right shoulder, and left ankle
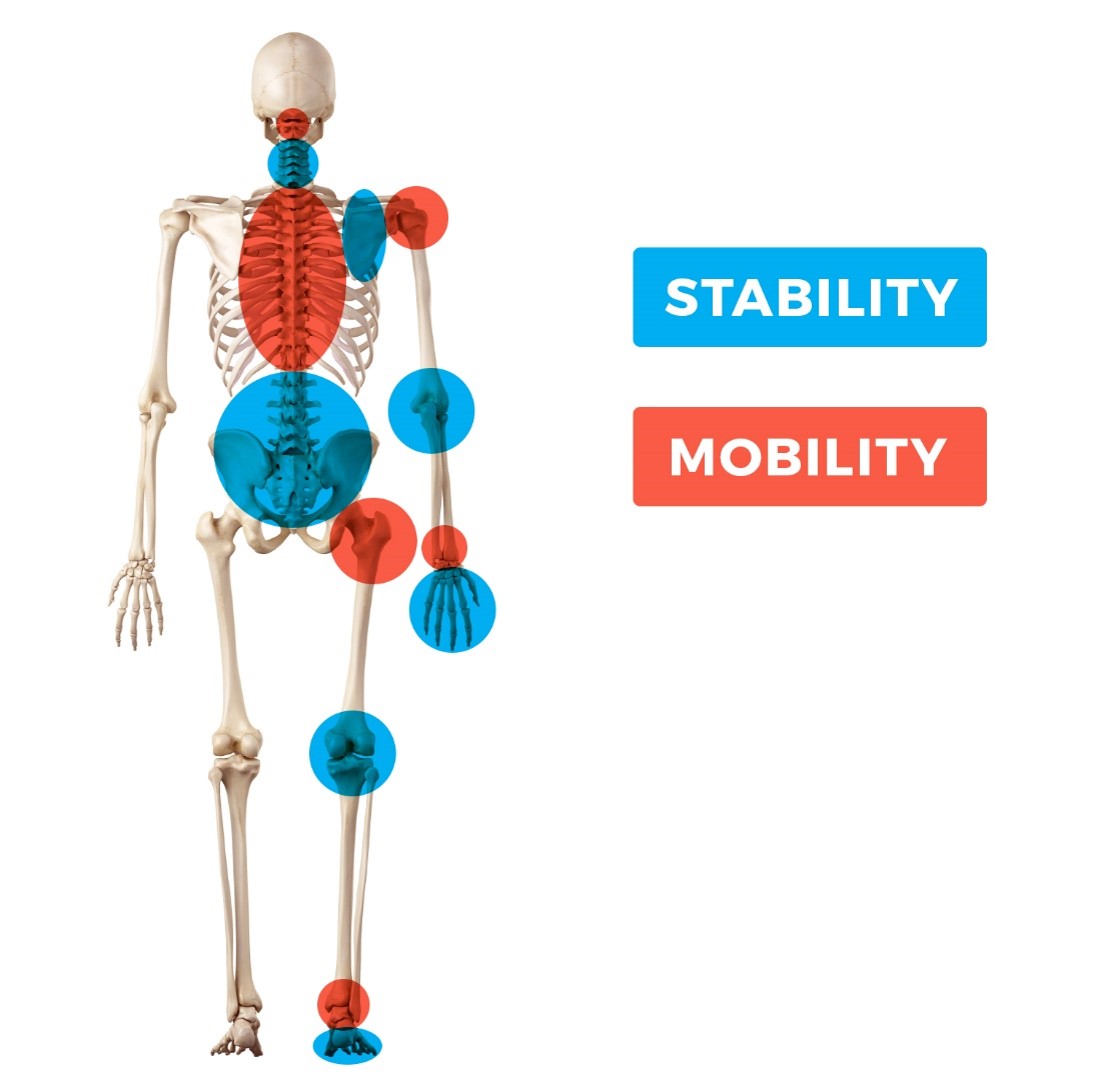 Generally after I run the SFMA, I have a conversation with the individual as to why I may be looking at different areas then they expected. I explained the joint by joint approach to the human body and why I felt her ankle and thorax were the biggest areas of concern, also focusing on the positives such as her hips are moving quite well! She became quite emotional and commented that she was so thankful someone was looking at all of her. She’d been wanting someone to look at her ankle because she felt it might be a problem. We developed a plan of care based on her findings and saw a decrease in her symptoms after one session.
Generally after I run the SFMA, I have a conversation with the individual as to why I may be looking at different areas then they expected. I explained the joint by joint approach to the human body and why I felt her ankle and thorax were the biggest areas of concern, also focusing on the positives such as her hips are moving quite well! She became quite emotional and commented that she was so thankful someone was looking at all of her. She’d been wanting someone to look at her ankle because she felt it might be a problem. We developed a plan of care based on her findings and saw a decrease in her symptoms after one session.Author
 Michele Desser is a Certified Athletic Trainer and serves as the Director of Education at Functional Movement Systems. She comes from a strong background of injury prevention, rehabilitation, movement assessment and performance training. Her expertise in the areas of movement assessment and correction, motor learning, strength development, and speed development allows her to help her clients achieve optimal mobility and stability patterns of movement. She has serves as an instructor for the SFMA and FMS curriculum and has been the training and movement assessment practitioner for the TPI Experience Team at the Titleist Performance Institute in Oceanside, CA. Michele received her Athletic Training education at the University at Buffalo.
Michele Desser is a Certified Athletic Trainer and serves as the Director of Education at Functional Movement Systems. She comes from a strong background of injury prevention, rehabilitation, movement assessment and performance training. Her expertise in the areas of movement assessment and correction, motor learning, strength development, and speed development allows her to help her clients achieve optimal mobility and stability patterns of movement. She has serves as an instructor for the SFMA and FMS curriculum and has been the training and movement assessment practitioner for the TPI Experience Team at the Titleist Performance Institute in Oceanside, CA. Michele received her Athletic Training education at the University at Buffalo.
Related Resources
Please login to leave a comment
1 Comments
-

David Hillmer 7/3/2023 8:51:44 AM
Hey Michele, thanks for sharing. Great article and always helpful to see/read that the standardized assessment (applied appropriately) leads to individual solutions for the client. Best regards from Germany, David