What I Look for in an FMS Score
Posted by Gray Cook
Imaging. X-Rays, MRI, Cat Scan, etc . . . love them or hate them, they are routine tools used by doctors in gathering information about a patient’s complaint. You can quickly search Google for articles on how imaging does not correlate with pain.

For example, in one study, 84% of those with no complaints of lower back pain had findings on imaging that normally would indicate pain/issues. However, these individuals had no pain or issues to report (1,2). Another study found shoulder abnormalities in 96% of the subjects using sonography, but they had no shoulder pain (3).
So it turns out that imaging is just information, and as Gray Cook explains, “Imaging should be used to confirm a diagnosis, not make one.”
But what does this have to do with Movement Screening and Exercise?
I’m getting there . . .
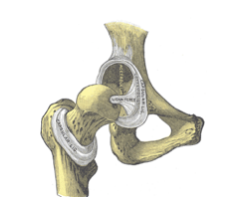
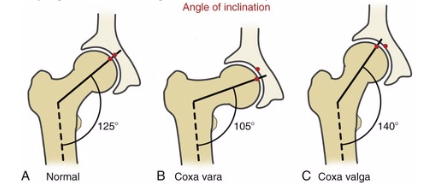
Hip labrum injuries, FAI (femoral acetabular impingement) and other hip issues have been increasingly diagnosed over recent years. And as a result, we have some interesting information from the imaging done in these situations. One study concluded that 87% of those with a Labrum tear or injury had a hip structural anomaly (4,5,6). Alpha angle, Coxa angle, Pincher style FAI, CAM style FAI, Retro-version, Ante-version and other hip structural anomalies are routinely found on imaging of those complaining of hip pain or issues (see pics at end of article).
This article by FMS Certified Ryan DeBell on “Why We Should All Squat Differently” does a solid job laying out hip variations that may impact how someone squats. There’s nothing like actually seeing the different shapes, angles and variations possible in the femoral head and neck to drive the point home that we all have our individual structural variations.
But again, what does this have to do with Movement Screening and Exercise?
I’m getting there . . .
First a personal story (my favorite kind). A few years ago, I embarked on a mission to increase my hip internal rotation range of motion. It was roughly zero. Seriously, about zero right and slightly more than zero on the left as measured by an SFMA Chiropractor I was seeing at the time. Despite being a 2 on my FMS DS, I decided that this glaring lack of a critical hip motion should be changed (look for my “learning” moment below). So, off I went stretching this and mobilizing that, and performing my squats and deadlifts and KB swings with my feet straight ahead.
The result . . . Hip pain and a trip to the doctor for an MRI arthrogram to get a good look at what was happening in my right hip. The pinch and pain had gotten pretty serious.
The result . . . A 61-degree Alpha angle and CAM-type FAI.
No joint degeneration in the acetabulum, complete tear of the anterior labrum and torn anterior superior labrum with two paralabral cysts (3 mm and 5 mm in size).
Anything over 49 degrees is considered clinically significant for Alpha Angle (a measure of when your femoral head changes shape) and I was at 61-degrees on the right and estimated 55-57 degrees on the left.
You see, through my previous exercise, I used a generous foot turn out for squatting, deadlifting etc., but once I began to target my hip internal rotation and perform my exercises with my feet straight ahead, I began to run into pinching and pain at the hip. That stress ultimately created the damage that the tests revealed.
Ah-ha moment revealed: Go back to the beginning of the paragraph here and reread my FMS DS score of 2 (and I could bore you with my other scores – all being symmetrical 2’s or better). My body had adjusted well around my structural “issue” as shown by my FMS score.
And now we come to it . . .
What does this all have to do with Movement Screening and Exercise?
In a nutshell, it means that movement screening and exercise play by different rules.
For movement screening (FMS), we use a consistently repeatable set-up for each screen. The DS uses a feet straight ahead position, HS has the feet together touching the test kit, and the ILL has the feet straight and in-line. All of these starting positions are critical to the FMS being a consistent and repeatable tool. These postures and positions confine you in movement screening to reveal the compensations. For exercise, we use individually determined foot positions that allow the individual to achieve their best form and safety.

It would be easy to look at the information on hip variation and my personal story and conclude that we should allow individual foot position, etc. for movement screening, but that would eliminate the reliability and utility of the FMS. And as I stated earlier, I was just fine on my FMS prior to deciding that a single range of motion was more important. The power of the FMS is not only the consistency and repeatability, but also the focus on patterns over parts for setting a baseline. Focusing on patterns over parts allows for individual adjustment and variation and is the reason scores of 2 on the FMS are totally adequate. The range of movement possible within a score of 2 allows for individual variation at an acceptable level. Fall into a range of 1’s or have zero, and you have entered a range of scores where I need to know why you have pain during a movement pattern (zero) or cannot access that pattern (1’s). It could easily be a structural issue that we cannot change or it could be an easily addressed movement issue, etc.
So use the verbal instructions, and set-up criteria strictly according to the “book,” but allow individual variation during exercise. As a starting point for foot position for exercise, check out the video on the “Lock and Rock” drill for finding individual foot placement.
Movement Screening is movement screening and exercise is exercise. Let them both play by their own rules and optimize both.
Brett Jones, Chief SFG, is a Certified Athletic Trainer and Strength and Conditioning Specialist based in Pittsburgh, PA. Mr. Jones holds a Bachelor of Science in Sports Medicine from High Point University, a Master of Science in Rehabilitative Sciences from Clarion University of Pennsylvania, and is a Certified Strength & Conditioning Specialist (CSCS) from the National Strength and Conditioning Association (NSCA).
With over twenty years of experience, Brett has been sought out to consult with professional teams and athletes, as well as present throughout the United States and internationally.
As an athletic trainer who has transitioned into the fitness industry, Brett has taught kettlebell techniques and principles since 2003. He has taught for Functional Movement Systems (FMS) since 2006, and has created multiple DVDs and manuals with world-renowned physical therapist Gray Cook, including the widely-praised “Secrets of…” series.
Brett continues to evolve his approach to training and teaching, and is passionate about improving the quality of education for the fitness industry. He is available for consultations and distance coaching by e-mailing him at appliedstrength@gmail.com. Follow him on Twitter at @BrettEJones
(1) Matsumoto, M., Okada, E., Toyama, Y., Fujiwara, H., Momoshima, S., & Takahata, T. (2013). Tandem age-related lumbar and cervical intervertebral disc changes in asymptomatic subjects. European Spine Journal, 22(4), 708-713.
http://doi.org/10.1007/s00586-012-2500-z
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3631032/
(2) Jensen, M. C., et.al (1994). Magnetic Resonance Imaging of the Lumbar Spine in People Without Back Pain. New England Journal of Medicine, 331(200), 69-73.
(3) Girish, G., et.al (2011, October 11). Ultrasound of the Shoulder: Asymptomatic Findings in Men. American Journal of Roentgenology, 197(4).
http://www.ajronline.org/doi/abs/10.2214/AJR.11.6971
(4) Wenger, D., Kendell, K., Miner, M., & Trousdale, R. (2004, September). Acetabular Labral Tears Rarely Occur in the Absence of Bony Abnormalities. Clinical Orthopaedics & Related Research, 426, 145-150. Retrieved from http://journals.lww.com/corr/Abstract/2004/09000/Acetabular_Labral_Tears_Rarely_Occur_in_the.24.aspx
(5) Ochoa, L., Dawson, L., Patzkowski, J., & Hsu, J. (2010, October). Radiographic Prevalence of Femoroacetabular Impingement in a Young Population with Hip Complaints Is High. Clinical Orthopaedics & Related Research, 468(10), 2710-2714. Retrieved from: 10.1007/s11999-010-1233-8.
(6) Kapron AL, Anderson AE, Aoki SK, et al. Radiographic Prevalence of Femoroacetabular Impingement in Collegiate Football Players: AAOS Exhibit Selection. ibid. 2011;93:e
Posted by Gray Cook
Posted by Brett Jones
Posted by Dr. Lee Burton
Ahhhh! I like it! First the "Brettzell." Now the "Lock and Rock"!
It sounds as though the screen is missing something if you have 0 degrees
Andre - not at all